International Community of Women Living with HIV Eastern Africa made a submission to the Family Planning (FP) 2020 Rights and Empowerment Working Group on Hormonal Contraception and HIV Risk.
Contact person
Ms. Lillian Mworeko
Regional Coordinator
International Community of Women Living with HIV Eastern Africa (ICWEA)
Plot 1106, Ssenge Road – Wakiso District
P.O. Box 32252, Kampala – Uganda
Tel: +256 4141531913/ 039
1.0 Introduction
The International Community of Women living with HIV Eastern Africa (ICW-EA) is a legally registered regional advocacy network and membership based organization founded by and for women living with HIV (WLHIV) in 2005 that exists to give visibility to WLHIV. ICWEA believes that gender inequalities and the limited access to sexual and reproductive health and rights for women are at the heart of the HIV epidemic. Our advocacy is based on evidence of our daily lived experiences.
In late 2011, ICW-EA decided that it was critical to begin to develop evidence-based advocacy at country and global level, reflecting women’s concerns with the open questions regarding the data on hormonal contraceptives and HIV in partnership with AVAC. This was based on the fact that data from a study published on October 4th 2011 in the Lancet suggested that use of hormonal contraceptives increases both the risk of acquiring and transmitting HIV—with the highest risk seen in those using the injectables depot-medroxyprogesterone acetate (DMPA) commonly known as depoprovera. The data came from two prospective studies of HIV incidence in HIV sero-discordant couples (one partner is HIV-negative, one is HIV-positive) in East and Southern Africa. The majority of couples in the cohort were part of the Partners in Prevention HSV/HIV Transmission Study, which looked at HSV-2 suppression and HIV transmission risk. Data from this cohort, along with data from couples enrolled in a separate observational study at Partners’ trial sites, were analyzed regarding hormonal contraceptives and HIV risk.
ICWEA acknowledges that family planning is a very important aspect of reproductive health given that it enhances women’s health. However, women need to make an informed decision while choosing which family planning method to use.
2.0 Our concerns for consideration by the members of FP2020 Rights and Empowerment Working Group
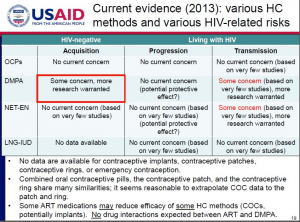
Current data leave unanswered questions about the link between hormonal contraceptives and women’s risk of acquiring HIV. The World Health Organization’s Technical Note on Hormonal Contraceptives and HIV states that these methods can be used without restriction but also states that, “Because of the inconclusive nature of the body of evidence on possible increased risk of HIV infection, women using progestogen-only contraception should be strongly advised to always use condoms, male or female, and other HIV preventive measures.”
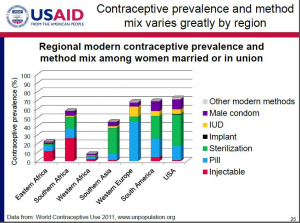
Progestogen-only contraceptives like Depo-Provera (also known as DMPA) are widely used, therefore we know more about them; we are starting to learn about other long-acting methods, including injectables and implants with different doses and types of synthetic hormones, which appear safer. This issue is highly relevant to women using family planning in sub-Saharan Africa. Among women using family planning in sub-Saharan Africa, 60 percent use Depo-Provera.
In spite of this uncertainty, most sub-Saharan African women aren’t receiving more options or more information. In the two years since WHO issued this technical note, there has been no communications training or guidance from UNFPA, UNAIDS, WHO or other normative agencies for service providers to help them explain the risks and benefits, knowns and unknowns of different methods. (PEPFAR has issued a technical brief on the subject. )
South Africa’s recently updated Contraceptive Policy provides an example of how to act on the uncertainty. One key conclusion is: “In light of recent research relating to the possible increased risk of HIV acquisition with injectable progestins, emphasis has shifted from injectable progestins to alternative long-acting reversible contraceptives (IUD, IUS, sub-dermal implants), with particularly attention paid to the importance of condom use for women who choose to use injectable progestins.”The country recently rolled out the subdermal implant as an alternative long-acting method.
There are other options. Compared to DEPO, there is less uncertainty about HIV risk associated with other long-acting family methods. The copper intra-uterine device (IUD) does not contain hormones. There is new data suggesting that women using NET-EN (another injectable method that lasts for two months and uses different hormones compared to Depo-Provera, which lasts three months) were not at increased risk, compared to women using Depo-Provera.
We don’t have to wait for more research to act. The question of whether Depo-Provera increases HIV risk has not been answered conclusively. The current uncertainty, combined with the unpopular side effects and the range of options that appear to carry less risk, support shifting away from Depo now, without waiting for more research. As this shift occurs, it will be possible to gather additional information on newer methods through well-designed observational studies and, perhaps, a randomized controlled trial.
This affects a limited number of countries. This is not a global shift. It is a matter of strategic action in the countries where both HIV prevalence and incidence and Depo Provera use are high:
Taking action is feasible and a “win-win” step. Countries like South Africa and Zimbabwe have already taken action with updated Contraceptive Policies that proactively seek to expand method mix in ways that will benefit all women, and address the unanswered questions related to DEPO and HIV risk.
Family Planning 2020 (FP2020) has a key leadership role to play. This initiative can play an instrumental role in expanding method mix in the key sub-Saharan African countries where HIV incidence and prevalence and DEPO use are all high. Recommendations to follow South African and Zimbabwean examples, building in strong monitoring of uptake and safety of new methods, will benefit millions of women.
This is an equity issue.Women in sub-Saharan Africa have the right to a wider array of safe, long-acting family planning methods that address concerns about HIV prevention and preventing unintended pregnancies.
3.0 Key recommendations for FP2020 Rights and Empowerment Working Group:
Be a strong voice for proactive change in the small number of countries with high HIV incidence, prevalence and Depo-Provera use. This change can be achieved through:
o Clear public leadership on the need to act on the persistent doubt about the link between specific hormonal contraceptives and HIV risk—taking action is feasible. FP2020 can use its resources and visibility for great benefit.
o Technical and financial support for countries to expand method mix—including national plans that follow the example/principles outline in South Africa’s plan, and set concrete uptake targets for women choosing long-acting methods other than Depo-Provera
o Participation in ongoing efforts to define a research agenda on HC-HIV that answers the questions of greatest relevance in a timely manner